Introduction – Vaccinations Save Lives
Vaccinations have saved more lives than any other health intervention, second only to clean water access[i]. Immunisation programs have dramatically decreased mortality from diseases worldwide and in Australia. Including reducing death from Diphtheria, Pertussis, and Tetanus (Figure 1). For example, a vaccination program against Diphtheria was introduced to Australia in the 1920s to 1930s[ii]. At this time, there was an average of 407 deaths per year. After the program’s introduction, there was a 40 per cent decrease in deaths from Diphtheria in one decade, followed by an average of five annual deaths three decades later. Australia reached zero deaths from Diphtheria in 1996. There was a lapse in time before immunisation had full protective effect on the population, because high vaccination rates are necessary to create population immunity. Individual immunisation is not as effective in reducing an individual’s risk of contracting the disease as vaccination of a large percentage of the population.
Figure 1: Decrease in disease mortality after introduction of vaccination programs
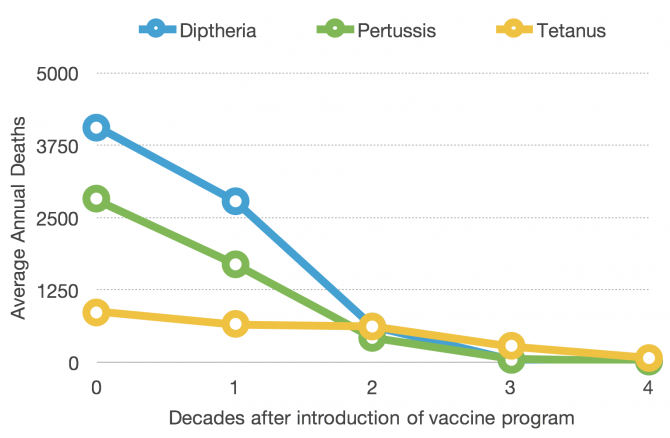
Source: National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases [iii]
High rates of immunisation are essential to protect the population from preventable diseases. 95 per cent of the population needs to be vaccinated to obtain herd immunity against a disease[iv]. Without herd immunity, a preventable disease may spread and infect the population. Vulnerable members of the society will be particularly at-risk, including young children and unborn babies who haven’t yet been vaccinated. Additionally, vaccines are not 100 per cent effective, meaning the whole population is at risk of contracting a disease if immunisation rates are low. When immunisation programs are compromised, disease outbreaks can occur causing mortality and a burden on the healthcare system. For example, there was a Pertussis outbreak in the United Kingdom due to an unfounded safety concern in 1976. The repercussions lasted 12 years, and resulted in a decrease of immunisation rates of up to 50 per cent, leading to 300,000 Pertussis notifications and at least 70 unnecessary deaths[v]. More recently, North America experienced a Measles outbreak due to an unfounded fear that the Measles-Mumps-Rubella (MMR) vaccine causes autism. In 2014 and 2015, there were 900 Measles cases in the United States and 322 cases in Canada due to the outbreak. Canada considered measles to be almost eradicated, however the resurgence of the disease could be attributed to a decrease in vaccination rates.
Australia’s national ‘Immunise Australia Program’ subsidises vaccines for eligible persons according to the National Immunisation Program (NIP) schedule[vi]. The program funds for vaccines against 14 diseases in children under 4 years, three in children 10 to 15 years, three in adults over 65 years, and a number of vaccines for at-risk populations such as Aboriginal and Torres Strait Islanders, and pregnant women. Australia’s immunisation program is complemented with policies to encourage vaccination, such as ‘No Jab, No Pay’. The efforts to increase vaccination rates are important, but need to expanded and constantly updated, to protect the Australian population from diseases.
Australian immunisation rates need to be increased in children, the elderly, and refugees
Australians are not at herd immunity levels for any of the vaccinations in the NIP. Australia is close to herd immunity levels in children, yet have a long way to go for other groups such as adults and refugees. The number of unvaccinated children is relatively small compared with the elderly population (Figure 1), and a relatively low percentage compared with refugees and the elderly (Figure 2). The national policies of the past ten years have a disproportionately high focus on child immunisation, with only two major policies focusing on the elderly, and none focusing on refugees[vii]. While child immunisation should remain a focus, the Federal Government also needs to give attention to other groups such as refugees and the elderly population.
Figure 2: Under-immunised populations in Australia

Source: Population numbers are from the Department of Immigration and Border Protection[viii], Australian Institute of Health and Welfare [ix], and Australia Bureau of Statistics [x]. Immunisation levels are from Immunise Australia Program [xi], Australian Institute of Health and Welfare[xii], and World Health Organisation[xiii].
Note: This is only an indication of the proportions of under-vaccination, as data on under-vaccination is from different years, and the vaccination coverage of adults and refugees are estimates from surveys and country-of-origin coverage data.
Figure 3: Immunisation coverage in Australia per sub-population
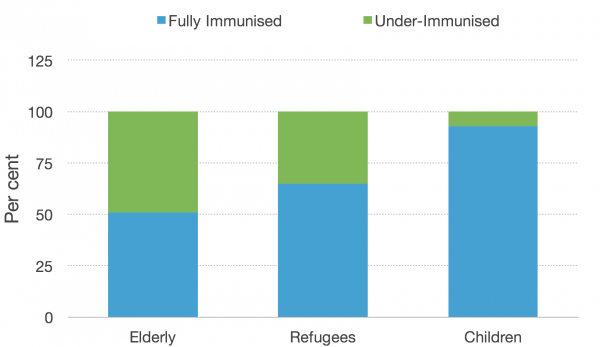
Source: Immunise Australia Program [xiv], Australian Institute of Health and Welfare[xv], and World Health Organisation[xvi]
Child Immunisation
93 per cent of young children are fully immunised for the NIP schedule[xvii]. Child immunisation rates are above 90 per cent in Australia due to a long history of focus on this area, with a multitude of approaches to increase immunisation. Past initiatives include the childhood immunisation register, free vaccinations, financial incentives for parents and immunisation providers, media campaigns, coercive policies, informational resources for providers and parents, and vaccination programs in various settings[xviii]. The regular introduction of new policies will continue to increase those levels.
During this, we need to ensure there is not an over-emphasis on anti-vaccination sentiments, as other reasons exist for under-vaccination of children. Currently, vaccine hesitancy is receiving a disproportionate amount of attention. A survey of 2,000 parents with young children in January, 2017, indicated that there were a multitude of reasons for under-vaccination (Table 1). The highest self-reported reason was a delay in their child’s vaccination due to an unrelated illness- a temporary reason. The second largest was anti-vaccination sentiments and vaccine doubts. Thirdly, logistical barriers included it being “too difficult to attend” vaccination sessions for their children, such as problems accessing a clinic in opening hours, and being unaware where to get free vaccinations for their children[xix]. Another barrier to vaccination was being born overseas and needing catch-up vaccines, which are available for children under 10 years permanently, and under 19 years until the end of 2017[xx].
Table 1: Parent’s self-reported reasons for under-vaccination of Australian children
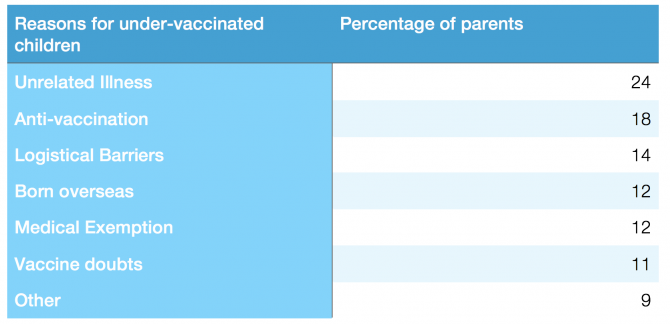
Source: ‘Vaccination: Perspectives of Australian Parents’ (2017) Child Health Poll
As Table 1 shows, anti-vaccination sentiments are prevalent in Australian parents, which increases the risk of low vaccination rates. Most anti-vaccination stances revolve around safety concerns with vaccinations that have been disproven, or pose less of a threat than abstaining from the vaccine. For example, the survey in 2017 found that 9 per cent of children’s parents believed vaccines caused autism, and 30 per cent were unsure if vaccines could cause autism[xxi]. This is an unfounded concern, as this link has been disproven by research. And the original publication that claimed a link between the MMR vaccine and autism in 1998, has been retracted and discredited as invalid and unethical[xxii]. Yet the public is still concerned with this link. Parental concern about vaccinations is unfortunately high. Reported conscientious objections for child vaccinations have increased steadily in Australia. In 1999, 0.23% of Australian children had recorded conscientious objections for vaccination, which has increased to 1.34% in 2015[xxiii]. Increasing anti-vaccination sentiment risks a future decrease in immunisation coverage, or an impeded increase in immunisation rates. Due to this, it is important to address anti-vaccination sentiments in Australia.
Recent national policies such as ‘No Jab, No Pay’, funded catch-up vaccines for those under 19 years, and a recently announced $5 million communication campaign all have a focus on vaccine-objectors, and on ‘vaccine hesitant’ parents. A GP communication strategy is also in development, to train GPs to effectively communicate with parents with vaccine doubts[xxiv]. The Federal Government’s focus is largely on ‘vaccine doubts’ and ‘anti-vaccination’ reasons from Table 1. The other reasons for under-vaccination are being neglected, leaving a gap in immunisation policy, and disadvantaging some children.
Vaccine objection is an important issue in child vaccination, however it is important to recognise that there are other factors that threaten immunisation rates that can be modified, such as practical barriers (Table 1). Parents that have practical barriers to their child’s vaccination need a different approach than vaccine objectors to increase immunisation levels. 14 per cent of un-vaccinating parents in the 2017 survey reported practical barriers. From 2012 to 2013, 3.4 per cent of Australian children were under-immunised but were not recorded objectors[xxv]. A large proportion were from the lowest 10 per cent of socioeconomic postcodes. This group of children are under-vaccinated for three suggested reasons: their parents did not record their vaccine objections, their vaccinations were not properly recorded in the national childhood register, or there was an access problem relating to logistical barriers, socioeconomic disadvantage, or access to healthcare[xxvi]. Children of these parents are disadvantaged from the financial punishment that their parents receive under ‘No Jab, No Pay’[xxvii]. To combat this, policies that focus on other problems such as logistical barriers are necessary, as well as policies targeted at anti-vaccination parents, such as No Jab, No Pay[xxviii].
Elderly immunisation
The elderly population are an important target for increasing immunisation rates as they are vulnerable to common, preventable diseases such as influenza. Adults have much lower rates of immunisation than children, as they have not been a focus of policy or the media. The NIP subsidises three vaccines for elderly Australians. Australians over 65 years of age are funded for the influenza vaccine once per year, the pneumococcal vaccine once every five years. Those aged 70 years are eligible for one shingles vaccine[xxix].
Immunisation of the elderly needs to be increased to decrease mortality and the burden on the healthcare system. Influenza can cause serious complications and death for the elderly population. An estimated 3,000 Australians over 50 years die each year from influenza and related complications[xxx]. Elderly hospital and GP visits due to influenza cost almost $80 million from 1998 to 2005[xxxi]. Additionally, about half of those over 85 will develop shingles in their life[xxxii].
There is a lack of accurate data on immunisation of the Australian elderly, making an increase in immunisation coverage challenging. A national whole-of-life register was introduced at the end of 2016 to remedy this[xxxiii]. However, to get the full benefit of the register, we need to ensure that immunisation providers are motivated to enter data. Due to the lack of sufficient data on the registry, we must rely on large surveys of the population to estimate levels of elderly immunisation. A survey estimated that only 51 per cent of elderly Australians were vaccinated against influenza and pneumococcal in 2009[xxxiv]. This survey is almost ten years old, and relies on the self-reporting of the elderly. The shingles vaccine was added to the list of funded vaccines in November 2016, and there is no sufficient data on the coverage rates of this vaccine. There is an absence of information on elderly vaccination, and this creates difficulty in accuracy of immunisation strategies to increase elderly vaccination.
Refugees
Australian refugees have lower immunisation rates than the Australian population, leaving them vulnerable to preventable diseases, and reducing Australia’s likelihood of herd immunity. There is a lack of data on immunisation coverage of refugees in Australia, which may be improved by the new whole-of-life register. However, refugees have had a disruption of their normal life, and most countries of origin do not have a comprehensive immunisation schedule, or have had a disruption that decreased vaccination opportunities for citizens[xxxv]. For example, the top five countries from which Australia received refugees in 2014 to 2015 had an estimated 13 to 37 per cent lower immunisation coverage than Australia (Table 1). Syria’s overall levels of immunisation have dropped from 86 per cent in 2010, to an estimated 56 per cent in 2016, due to the disruption of the Syrian civil war[xxxvi].
Table 2: Country of Origin and their Immunisation rates for Humanitarian Visas
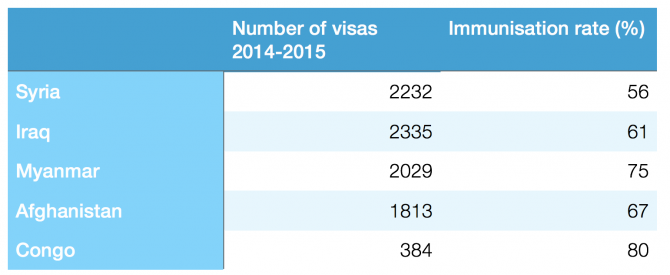
Source: World Health Organisation and Department of Immigration and Border Protection
Syrian and Iraqi refugees are our largest refugee intake, and have very low levels of immunisation. Syrian and Iraqi refugees were granted 8,640 Australian humanitarian visas from 2015 to 2016[xxxvii]; 62 per cent of the granted visas for that period[xxxviii]. In 2017, there will be 12,000 additional humanitarian visas provided to Syrian and Iraqi refugees[xxxix]. Their levels of under-vaccination leave them at risk of catching diseases, as well as increasing Australia’s vulnerability to preventable diseases. For example, Australian cases of congenital Rubella infection are almost all due to under-immunised mothers born overseas[xl]. Congenital Rubella is caused by Rubella infection of the mother during pregnancy, and can result in foetal death, blindness, deafness or cardiac problems. Immunisation against Rubella is provided free-of-charge for young Australian children. Adult refugees may not have the same access to vaccination programs in their country of origin.
The NIP does not subsidise vaccines for adult refugees. States provide some funded vaccinations for refugees, but this is inconsistent from state-to-state, as the Commonwealth does not provide funding for refugee immunisation programs. For example, NSW funds three of the 16 vaccines that are funded by the National Immunisation Program[xli]. All refugee children receive free vaccination as per the Immunise Australia Program for all Australian children[xlii].
Overcoming the Challenge
Recommendations:
- The Federal Health Department should use their new area-based campaign to identify area-specific vaccination barriers, and not assume a blanket approach addressing vaccine myths will work to increase immunisation rates in every area.
- The Federal Government should introduce a financial incentive for immunisation providers to enter data into the whole-of-life resister about NIP-funded adult vaccination.
- The Federal Government should fund a national catch-up vaccine program for refugees.
The new campaign should determine area-specific reasons for under-vaccination
The Federal Government has introduced a $5 million communication campaign that will end in 2019[xliii]. The campaign will focus on the areas with the lowest immunisation in Australia, with an emphasis on de-bunking vaccination myths. The campaign will reach 11,000 childcare centres across the country, and use doctors and social media as ways to reach parents of young children. An area-based campaign is necessary, as there are areas with immunisation rates far below the national level[xliv]. However, the campaign developers should identify vaccination barriers in under-immunised areas, and should not assume all parents of under-vaccinated children are vaccine-hesitant or vaccine objectors.
A blanket approach that focuses solely on vaccine myths will not work to increase immunisation rates in every area. The campaign aims to address “myths and misconceptions”[xlv] in areas of low immunisation, however not every area’s low immunisation will be due to vaccine objections. An area’s low immunisation rates may be explained by alternate reasons (Table 1). These groups need a policy that does more than dispel myths on the safety of vaccinations.
World Health Organisation Europe’s tailored approach suggests identifying specific barriers within high-risk areas[xlvi]. The approach suggests gathering information from the vaccine providers and parents in the area about the reasons for under-vaccination. By focusing on specific childcare centres, the new campaign has the potential to conduct research and determine centre-specific reasons for under-vaccination. The extra effort of finding out the area-specific reasons for low immunisation would lead to a tailored, most likely more effective campaign.
Immunisation providers should receive a payment for adding adult vaccination data to the new whole-of-life register
To increase immunisation levels in Australia, the Federal Government needs to ensure that immunisation of the elderly is properly recorded in the new whole-life-register. A whole-of-life register was introduced in 2016 to record adult immunisation, known as Australian Immunisation Register (AIR). This is an important step in increasing elderly immunisation, as surveillance and comprehensive data is essential to a successful immunisation program[xlvii]. The register will allow knowledge of individual patient immunisation status, immunisation of the population, and areas that need improvement. For example, the register for childhood vaccination allowed the development of a campaign to target areas with low vaccination rates. To have such focus in adult immunisation, comprehensive data on the whole-of life-register is important.
To encourage comprehensive data collection, doctors should be incentivised to enter data about NIP-funded adult vaccinations. When the childhood register was released in 1996, there was a national $6 payment for each entry into the register of a NIP funded vaccination, and a $3 payment in Queensland[xlviii]. Currently, there are two $6 payments offered to doctors for data entry about children immunisation; one for notifying that a child under 7 has been fully immunised, and one for notification of a catch-up vaccination for a child who was more than 2 months behind the schedule[xlix]. The Federal Government should introduce a payment for notification of immunisation of an elderly patient.
Up to 98 per cent of Australian health professionals are in support of adult immunisation[l]. However, the introduction of a new register creates more work for immunisation providers. There are often more pressing matters when an elderly person is in a health care setting, and preventative health care may seem unimportant in contrast[li]. To make elderly immunisation a priority, the Federal Government should pay doctors an equivalent payment for adult immunisation notification as they receive for child immunisation notification.
Refugees should receive a free catch-up immunisation program
The lack of immunisation in refugees leaves this group at higher risk of contracting disease, and decreases Australia’s protection against vaccine-preventable diseases. To combat this, the Australian National Health Department should provide refugees the same access to vaccinations that other Australians receive solely due to their birthplace. Australian-born citizens receive 14 free vaccinations as young children, and 5 vaccinations at school age[lii]. Refugees deserve a catch-up program that funds all of these vaccines.
The Immunisation Australia Program’s stated objectives include: “identify cohorts of low coverage and implement strategies to improve immunisation coverage”, and “ensure equity of access to immunisation services for all Australians regardless of financial or geographical barriers.”[liii]. These objectives justify a funded catch-up program for refugees to have equal access to vaccines that Australian-born citizens have. Reducing out-of-pocket costs of vaccines has been proven to be an effective strategy in increasing immunisation rates in contexts such as adult and child immunisation[liv] [lv].
The cost to fund catch-up vaccines for refugees will be proportionately small compared to immunisation of Australian children. There are approximately 13,000 refugees arriving in Australia each year[lvi]. In contrast, there were approximately 1.6 million children from 0 to 4 years old in Australia in June, 2015 to June, 2016[lvii]. If a catch-up was introduced for recent refugees, there would be 65,068 refugees since 2012 that could be eligible for the catch-up[lviii],[lix]. A catch-up scheme for refugees would cost relatively little and would increase immunisation coverage in Australia[lx].
Conclusion
Australia remains a leading immunisation nation. But in key demographic groups, improvements in the immunisation rate need to be improved to ensure Australia retains herd immunity from a range of significant illnesses. This report has identified how Australia’s immunisation rates could be increased through a combination of targeted approaches. Specifically, it has argued for the need to increase the protection of at-risk groups, such as under-immunised children, the elderly, and refugees against preventable disease.
The Federal Health Department’s new campaign should identify the specific vaccination barriers in under-immunised areas, and should not assume all parents of under-vaccinated children are vaccine objectors who need to hear about vaccine myths. Other reasons for under-immunisation include lack of access, low socioeconomic status, and different country of origin. The area-based campaign should draw on the World Health Organisation Europe’s tailored approach, and determine reasons for under-vaccination from parents and immunisation providers[lxi].
The Federal Government should introduce an incentive to encourage comprehensive data collection for immunisation of the elderly. The lack of data on elderly vaccination in Australia means that it is difficult to effectively create programs to increase immunisation coverage, and cannot monitor individual immunisation status. The Federal Government should introduce a $6 payment to doctors who enter data on NIP-funded elderly vaccination into the new whole-of-life register.
To increase immunisation levels in a vulnerable and at-risk group of the Australian population, the Federal Government should introduce a funded catch-up vaccine program for refugees. The population of refugees is under-vaccinated, and their immunisation will increase their protection against disease, increase Australia’s herd immunity, and increase equity.
Currently, anti-vaccination sentiments of young children’s parents receives disproportionate attention in Australia’s national immunisation policies. The Federal Government should focus more attention on other areas of weakness, such as children with under-vaccination due to practical barriers, and under-vaccination in the elderly and refugee populations[lxii]. This increased spread of focus will assist in increasing herd immunity levels and therefore increase Australia’s protection against vaccine-preventable diseases.
References
[i] Andre F, Booy R, Bock H, Clemens J, Datta S, John T, Lee B, Lolekha S, Peltola H, Ruff T, Santosham M, Schmitt H. (2008) Vaccination greatly reduces disease, disability, death and inequity worldwide. World Health Organisation. Retrieved from http://www.who.int/bulletin/volumes/86/2/07-040089/en/
[ii] Lawrence, G., Wang, H., Gilmour, R., Hull, B., Burgess, M., Gidding, H., . . . National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases. (2002). Vaccine preventable diseases and vaccination coverage in Australia, 1999 to 2000. Communicable Diseases Intelligence Quarterly Report, Suppl(2002 May), i-111. Retrieved from http://www.health.gov.au/internet/main/publishing.nsf/content/cda-pubs-cdi-2002-cdi26suppl-vpd99_00.htm/$FILE/vpd99_00.pdf
[iii] Lawrence, G., Wang, H., Gilmour, R., Hull, B., Burgess, M., Gidding, H., . . . National Centre for Immunisation Research and Surveillance of Vaccine Preventable Diseases. (2002). Vaccine preventable diseases and vaccination coverage in Australia, 1999 to 2000. Communicable Diseases Intelligence Quarterly Report, Suppl(2002 May), i-111. Retrieved from http://www.health.gov.au/internet/main/publishing.nsf/content/cda-pubs-cdi-2002-cdi26suppl-vpd99_00.htm/$FILE/vpd99_00.pdf
[iv] Gidding, H. F., Burgess, M. A., & Kempe, A. E. (2001). A short history of vaccination in Australia. The Medical Journal of Australia, 174(1),37.
[v] Nicoll, A., Elliman, D., & Ross, E. (1998). MMR vaccination and autism 1998: Déjà vu-pertussis and brain damage 1974? BMJ: British Medical Journal, 316(7133), 715-716.
[vi] Department of Health (2016) National Immunisation Program Schedule (From 20 April 2015) Australian Government. Retrieved from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/national-immunisation-program-schedule
[vii] National Centre for Immunisation Research and Surveillance (2016) Significant events in immunisation policy and practice* in Australia. Canberra, ACT: Australian Government. Retrieved from http://www.ncirs.edu.au/assets/Uploads/Immunisation-Policy-and-Practice-June-2016.pdf
[viii] Department of Immigration and Border Protection (2016) Annual Report 2015–16. Canberra, ACT: Australian Government. Retrieved from ISSN 2205-2089
[ix] Australian Institute of Health and Welfare (2011). 2009 Adult Vaccination Survey: summary results. Canberra, ACT: Australian Government. Retrieved from: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418286
[x] Australian Bureau of Statistics (2017) Feature article: population by age and sex, Australia, states, and territories (No. 3101.0). Canberra, ACT: Australian Government. Retrieved from: http://www.abs.gov.au/ausstats/abs@.nsf/0/1CD2B1952AFC5E7ACA257298000F2E76?OpenDocument
[xi] Department of Health (2017) AIR – Current Data. Canberra, ACT: Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/acir-curr-data.htm
[xii] Australian Institute of Health and Welfare (2011). 2009 Adult Vaccination Survey: summary results. Canberra, ACT: Australian Government. Retrieved from http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418286
[xiii] World Health Organisation (2017) WHO vaccine-preventable diseases: monitoring system. 2016 global summary. Retrieved from http://apps.who.int/immunization_monitoring/globalsummary/
[xiv] Department of Health (2017) AIR – Current Data. Canberra, ACT: Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/acir-curr-data.htm
[xv] Australian Institute of Health and Welfare (2011). 2009 Adult Vaccination Survey: summary results. Canberra, ACT: Australian Government. Retrieved from http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418286
[xvi] World Health Organisation (2017) WHO vaccine-preventable diseases: monitoring system. 2016 global summary. Retrieved from http://apps.who.int/immunization_monitoring/globalsummary/
[xvii] Department of Health (2017) AIR – Current Data. Canberra, ACT: Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/acir-curr-data.htm
[xviii] National Centre for Immunisation Research and Surveillance (2016) Significant events in immunisation policy and practice* in Australia. Canberra, ACT: Australian Government. Retrieved from http://www.ncirs.edu.au/assets/Uploads/Immunisation-Policy-and-Practice-June-2016.pdf
[xix] Rhodes A., (2017) Vaccination: Perspectives of Australian parents. Australian Child Health Poll, The Royal Children’s Hospital Melbourne. Retrieved from: https://www.childhealthpoll.org.au/wp-content/uploads/2017/03/ACHP-Poll6_Detailed-report_FINAL.pdf
[xx] Department of Health. (2016) No Jab, No Pay – New Immunisation Requirements for Family Assistance Payments. Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/67D8681A67167949CA257E2E000EE07D/$File/No-Jab-No-Pay-FSheet.pdf
[xxi] Rhodes A. (2017) Vaccination: Perspectives of Australian parents. Australian Child Health Poll, The Royal Children’s Hospital Melbourne. Retrieved from: https://www.childhealthpoll.org.au/wp-content/uploads/2017/03/ACHP-Poll6_Detailed-report_FINAL.pdf
[xxii] King, C., & Leask, J. (2017). The impact of a vaccine scare on parental views, trust and information needs: A qualitative study in Sydney, Australia. BMC Public Health, 17(1) doi:10.1186/s12889-017-4032-2
[xxiii] Department of Health (2016) No Jab, No Pay- New Immunisation Requirements for Family Assistance Payments. Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/67D8681A67167949CA257E2E000EE07D/$File/No-Jab-No-Pay.pdf
[xxiv] National Centre for Immunisation Research and Surveillance (2016) The SARAH project: supporting vaccination discussions between parents and health professionals. Retrieved from: http://www.ncirs.edu.au/research/social-research/sarah-project/
[xxv] Beard, F. H., Hull, B. P., Leask, J., Dey, A., & McIntyre, P. B. (2016). Trends and patterns in vaccination objection, Australia, 2002-2013. The Medical Journal of Australia, 204(7), 275.
[xxvi] Leask, J. and Danchin, M. (2017), Imposing penalties for vaccine rejection requires strong scrutiny. J Paediatr Child Health, 53: 439–444. doi:10.1111/jpc.13472
[xxvii] Booy R. (2017) Personal interview.
[xxviii] Leask, J. and Danchin, M. (2017), Imposing penalties for vaccine rejection requires strong scrutiny. J Paediatr Child Health, 53: 439–444. doi:10.1111/jpc.13472
[xxix] Department of Health (2016) National Immunisation Program Schedule (From 20 April 2015) Australian Government. Retrieved from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/national-immunisation-program-schedule
[xxx] Newall, A. T., Wood, J. G., & MacIntyre, C. R. A. (2008). Influenza-related hospitalisation and death in Australians aged 50 years and older. Vaccine, 26(17), 2135-2141.
[xxxi] Newall, A. T., & Scuffham, P. A. (2008). Influenza-related disease: The cost to the Australian healthcare system. Vaccine, 26(52), 6818-6823. doi:10.1016/j.vaccine.2008.09.086
[xxxii] National Centre for Immunisation Research and Surveillance (2015). Zoster vaccine for Australian adults | NCIRS Fact sheet. Australian Government. Retrieved from http://www.ncirs.edu.au/assets/provider_resources/fact-sheets/herpes-zoster-vaccine-fact-sheet.pdf
[xxxiii] Department of Health (2016) Immunise Australia Program: Expansion of Registers. Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/expansion-registers
[xxxiv] Australian Institute of Health and Welfare (2011). 2009 Adult Vaccination Survey: summary results. Canberra, ACT: Australian Government. Retrieved from http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418286
[xxxv] Kpozehouen, E., Heywood, A. E., Kay, M., Smith, M., Paudel, P., Sheikh, M. and MacIntyre, C. R. (2017). Improving access to immunisation for migrants and refugees: recommendations from a stakeholder workshop. Australian and New Zealand Journal of Public Health, 41: 118–120. doi:10.1111/1753-6405.12602
[xxxvi] World Health Organisation (2017) WHO vaccine-preventable diseases: monitoring system. 2016 global summary. Retrieved from http://apps.who.int/immunization_monitoring/globalsummary/
[xxxvii] Department of Immigration and Border Protection (2017) Australia’s response to the Syrian and Iraqi humanitarian crisis. Australian Government. Retrieved from https://www.border.gov.au/Trav/Refu/response-syrian-humanitarian-crisis
[xxxviii] Department of Immigration and Border Protection (2016) Annual Report 2015–16. Canberra, ACT: Australian Government. Retrieved from ISSN 2205-2089
[xxxix] Department of Immigration and Border Protection (2017) Australia’s response to the Syrian and Iraqi humanitarian crisis. Australian Government. Retrieved from https://www.border.gov.au/Trav/Refu/response-syrian-humanitarian-crisis
[xl] Khandaker, G., Zurynski, Y., & Jones, C. (2014). Surveillance for congenital rubella in australia since 1993: Cases reported between 2004 and 2013. Vaccine, 32(50), 6746-6751. doi:10.1016/j.vaccine.2014.10.021
[xli]NSW Department of Health (2011) Refugee Health Plan 2011-2016. North Sydney: NSW Government. Retrieved from: http://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2011_014.pdf
[xlii] Department of Health (2016) No Jab, No Pay- New Immunisation Requirements for Family Assistance Payments. Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/67D8681A67167949CA257E2E000EE07D/$File/No-Jab-No-Pay.pdf
[xliii] Minister Hunt (2017). New campaign to encourage further childhood vaccination. [media release] Department of Health, Australian Government.
[xliv] Department of Health (2017) AIR – Current Data. Canberra, ACT: Australian Government. Retrieved from http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/acir-curr-data.htm
[xlv] Minister Hunt (2017). New campaign to encourage further childhood vaccination. [media release] Department of Health, Australian Government.
[xlvi] World Health Organisation (2013) The Guide to Tailoring Immunization Programmes (TIP) World Health Organisation: Regional Office for Europe. Retrieved from: http://www.euro.who.int/__data/assets/pdf_file/0003/187347/The-Guide-to-Tailoring-Immunization-Programmes-TIP.pdf
[xlvii] Henderson, D. A. (1999). Lessons from the eradication campaigns. Vaccine, 17, S53-S55. doi:10.1016/S0264-410X(99)00293-5
[xlviii]National Centre for Immunisation Research and Surveillance (2016) Significant events in immunisation policy and practice* in Australia. Canberra, ACT: Australian Government. Retrieved from http://www.ncirs.edu.au/assets/Uploads/Immunisation-Policy-and-Practice-June-2016.pdf
[xlix] Australian Immunisation Register for health professionals. https://www.humanservices.gov.au/health-professionals/services/medicare/australian-immunisation-register-health-professionals
[l] Ridda, I., Lindley, I. R., Gao, Z., McIntyre, P., & Madntyre, C. R. (2008). Differences in attitudes, beliefs and knowledge of hospital health care workers and community doctors to vaccination of older people. Vaccine, 26(44), 5633-5640. doi:10.1016/j.vaccine.2008.07.070
[li] Ridda, I., Lindley, I. R., Gao, Z., McIntyre, P., & Madntyre, C. R. (2008). Differences in attitudes, beliefs and knowledge of hospital health care workers and community doctors to vaccination of older people. Vaccine, 26(44), 5633-5640. doi:10.1016/j.vaccine.2008.07.070
[lii] Department of Health (2016) National Immunisation Program Schedule (From 20 April 2015) Australian Government. Retrieved from: http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/national-immunisation-program-schedule
[liii] http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/B2D3E81EEDF2346ACA257D4D0081E4BC/$File/nat-immune-strategy-2013-18-final.pdf
[liv] Yoo, B.-K., Berry, A., Kasajima, M., & Szilagyi, P. G. (2010). Association between Medicaid reimbursement and child influenza vaccination rates. Pediatrics, 126(5), e998-e1010. doi:10.1542/peds.2009-3514
[lv] Merkel, P. A., & Caputo, G. C. (1994). Evaluation of a simple office-based strategy for increasing influenza vaccine administration and the effect of differing reimbursement plans on the patient acceptance rate. Journal of general internal medicine, 9(12), 679-683. doi:10.1007/BF02599008
[lvi] Australian Bureau of Statistics (2017) Feature article: population by age and sex, Australia, states, and territories (No. 3101.0). Canberra, ACT: Australian Government. Retrieved from: http://www.abs.gov.au/ausstats/abs@.nsf/0/1CD2B1952AFC5E7ACA257298000F2E76?OpenDocument
[lvii] Australian Bureau of Statistics (2017) Feature article: population by age and sex, Australia, states, and territories (No. 3101.0). Canberra, ACT: Australian Government. Retrieved from: http://www.abs.gov.au/ausstats/abs@.nsf/0/1CD2B1952AFC5E7ACA257298000F2E76?OpenDocument
[lviii] Department of Immigration and Border Protection (2016) Fact sheet – Australia’s Refugee and Humanitarian programme. Canberra, ACT: Australian Government. Retrieved fromhttps://www.border.gov.au/about/corporate/information/fact-sheets/60refugee
[lix] Department of Immigration and Border Protection (2016) Annual Report 2015–16. Canberra, ACT: Australian Government. Retrieved from ISSN 2205-2089
[lx] Heywood, A. (2017) Personal interview
[lxi]World Health Organisation (2013) The Guide to Tailoring Immunization Programmes (TIP) World Health Organisation: Regional Office for Europe. Retrieved from: http://www.euro.who.int/__data/assets/pdf_file/0003/187347/The-Guide-to-Tailoring-Immunization-Programmes-TIP.pdf
[lxii] Rhodes A., (2017) Vaccination: Perspectives of Australian parents. Australian Child Health Poll, The Royal Children’s Hospital Melbourne. Retrieved from: https://www.childhealthpoll.org.au/wp-content/uploads/2017/03/ACHP-Poll6_Detailed-report_FINAL.pdf


SOCIAL SHARE